What Is The Thyroid Gland?
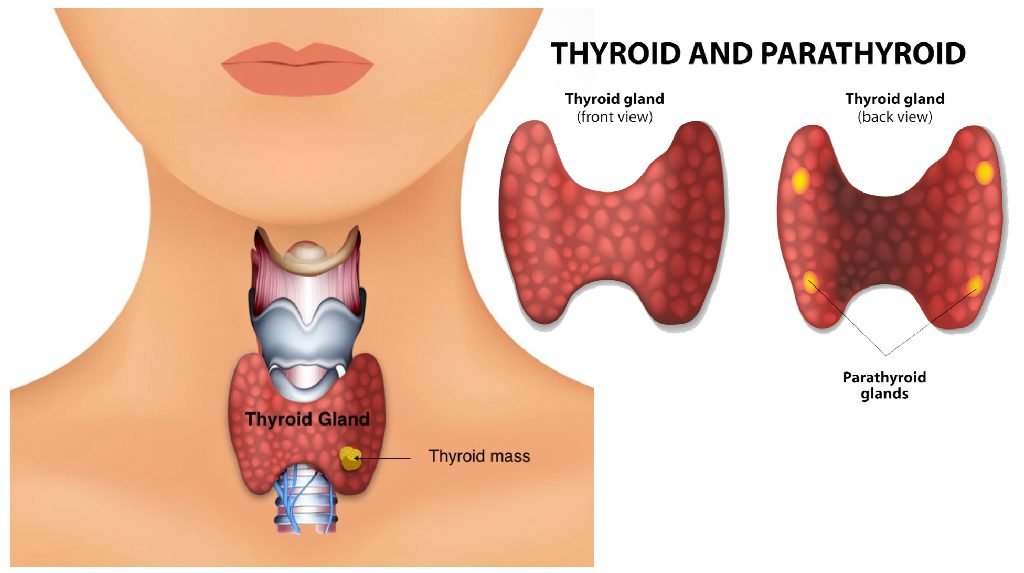
Butterfly-shaped endocrine gland that is normally located in the lower front of the neck. The thyroid function is to make thyroid hormones, which are secreted into blood and then carried to every cell. Thyroid hormone helps the body use energy, stay warm and keep the brain, heart, muscles, and other organs working normally.
Symptoms:
1. You may have thyroid cancer from the nodule you have.
2. Thyroid cancer has been diagnosed in you.
3. You have a goitre or nodule that is causing local symptoms, such as tracheal constriction, swallowing difficulties, or an unattractive or visible lump.
4. You have either Graves’ disease, a toxic nodule, or a toxic multinodular goitre that is producing and releasing too much thyroid hormone, resulting in symptoms.

The extent of your thyroid surgery should be discussed by you and your thyroid surgeon and can generally be classified as a partial thyroidectomy or a total thyroidectomy.
Removal of part of the thyroid can be classified as.
1. A hemi-thyroidectomy or thyroid lobectomy – where one lobe (one half) of the thyroid is removed.
2. An isthmusectomy – removal of just the bridge of thyroid tissue between the two lobes; used specifically for small tumours that are located in the isthmus.
3. Finally, a total or near-total thyroidectomy is the removal of all or most of the thyroid tissue. The recommendation as to the extent of thyroid surgery will be determined by the reason for the surgery. For instance, a nodule confined to one side of the thyroid may be treated with a hemi-thyroidectomy.For a large bilateral goitre or a large thyroid cancer, then you will probably have a recommendation for a total thyroidectomy. However, the extent of surgery is depends upon disease pattern.
Will I be able to lead a normal life after surgery?
- Yes. Once you have recovered from thyroid surgery, you will usually be able to do all activity do by you prior to surgery. Some patients become hypothyroid following thyroid surgery, requiring treatment with thyroid hormone. This is especially true if you had your whole thyroid gland removed. Generally, you will be started on thyroid hormone the day after surgery, even if there are plans for treatment with radioactive iodine
Why do I need an operation?
The most common reason for thyroid surgery is to remove a thyroid nodule, suspicious through a fine needle aspiration biopsy. Surgery may be recommended for the following biopsy results:
- Cancer (papillary cancer)
- Possible cancer (follicular neoplasm or atypical findings)
- Cosmetic purposes
- Molecular marker testing of biopsy specimen which indicates a risk for malignancy
- Surgery may be also recommended for nodules with benign biopsy results if the nodule is large, if it continues to increase in size or if it is causing symptoms (discomfort, difficulty swallowing, etc.). Surgery is also an option for the treatment of hyperthyroidism (Grave’s disease or a “toxic nodule” for large and multinodulargoitres and for any goitre that may be causing symptom
Are there other forms of treatment?
Surgery will be definitely indicated to remove nodules suspicious for thyroid cancer. In the absence of a possibility of thyroid cancer, there may be nonsurgical options for therapy depending on your diagnosis.
All patients considering thyroid surgery should be evaluated preoperatively with a thorough and detailed medical history and physical exam including cardiopulmonary (heart and lungs) evaluation. An electrocardiogram and a chest x-ray prior to surgery are often recommended for patients who are over 45 years of age or who are symptomatic from heart disease. Blood tests may be performed to determine if a bleeding disorder is present. Importantly, any patient who has had a change in voice or who has had a previous neck operation (thyroid surgery, parathyroid surgery, spine surgery, carotid artery surgery etc.)
This is necessary to determine whether the recurrent laryngeal nerves that control the vocal cord muscles are functioning normally. Finally, in rare cases, if medullary thyroid cancer is suspected, patients should be evaluated for endocrine tumours that occur as part of familial syndromes including adrenal tumours (pheochromocytomas) and enlarged parathyroid glands that produce excess parathyroid hormone (hyperparathyroidism)
What are the risks of the operation?
Thyroid surgery is generally very safe. Complications are uncommon, but the most serious possible risks of thyroid surgery include:
- Bleeding in the hours right after surgery that could lead to acute respiratory distress
- Injury to a recurrent laryngeal nerve that can cause temporary or permanent hoarseness and possibly even acute respiratory distress in the very rare event that both nerves are injured
- Damage to the parathyroid glands that control calcium levels in the blood, leading to temporary, or more rarely, permanent hypoparathyroidism and hypocalcemia.
These complications occur more frequently in patients with invasive tumours or extensive lymph node involvement, Overall the risk of any serious complication should be less than 2%. Prior to surgery, patients should understand the reasons for the operation, the alternative methods of treatment, and the potential risks and benefits of the operation (informed consent).
Will I need to take a thyroid pill after my operation?
The answer to this depends on how much of the thyroid gland is removed. If you have your entire gland removed (total thyroidectomy) or if you have had prior thyroid surgery and now are facing removal of the remaining thyroid (completion thyroidectomy) then you have no internal source of thyroid hormone remaining and you will definitely need lifelong thyroid hormone replacement.


 ACL Injury
ACL Injury Gall Bladder Stone
Gall Bladder Stone